The Vicious Cycle of Co-Occurring Disorders

Many people struggle with addiction. Even more face mental health challenges like anxiety or depression. We know these two issues often go hand-in-hand. This strong connection, called a co-occurring disorder, can make healing feel much harder.
But there is a brighter path forward.
In this comprehensive guide, we will explore integrated addiction and mental health treatment. This modern approach helps people heal from both problems at the same time. We will show you why this unified care is so important. We will cover its main parts and the many benefits it offers. Our goal is to help you understand how to find the right support for a complete and lasting recovery.
The landscape of addiction and mental health in the United States, and particularly in regions like Johnson City, TN, paints a concerning picture. According to the 2021 National Survey on Drug Use and Health (NSDUH), a staggering 44.1 million American adults reported a substance use disorder (SUD) in the past year. This widespread issue affects individuals from all walks of life, highlighting the urgent need for effective intervention and support.
Beyond the national figures, Tennessee faces its own unique challenges. The state has consistently ranked among the highest for prescription opioid abuse, a crisis that has profoundly impacted communities across the region. In 2017 alone, more than 6,879,698 painkiller prescriptions were written in Tennessee, a number that exceeded the state's population at the time. This over-prescription has fueled an opioid epidemic, leading to approximately 70,000 Tennessee residents currently suffering from some form of opioid addiction.
The consequences are dire. The number of drug overdoses in Tennessee rose from 1,818 in 2018 to 2,089 in 2019, reflecting a grim upward trend. Washington County, where Johnson City is located, has been particularly hard-hit, reporting the second-highest number of drug overdoses in the state. In 2018, the overdose rate due to fentanyl and other synthetic opioids reached 12.83 people per 100,000 in Washington County, underscoring the severity of the synthetic opioid crisis. These statistics are not just numbers; they represent lives lost, families shattered, and communities struggling to cope.
While opioids dominate the headlines, other substances also pose significant threats. Alcohol remains the most commonly abused substance in Johnson City, with the 2021 NSDUH indicating that 29.5 million people aged 12 and older reported alcohol abuse nationwide. This widespread alcohol use often co-occurs with mental health conditions, creating a complex web of challenges for individuals seeking recovery.
Mental health statistics further complicate the picture. Many individuals struggling with substance use also grapple with underlying mental health disorders such as depression, anxiety, PTSD, or bipolar disorder. When these two conditions—substance use disorder and a mental health disorder—occur simultaneously, they are referred to as co-occurring disorders, or dual diagnosis.
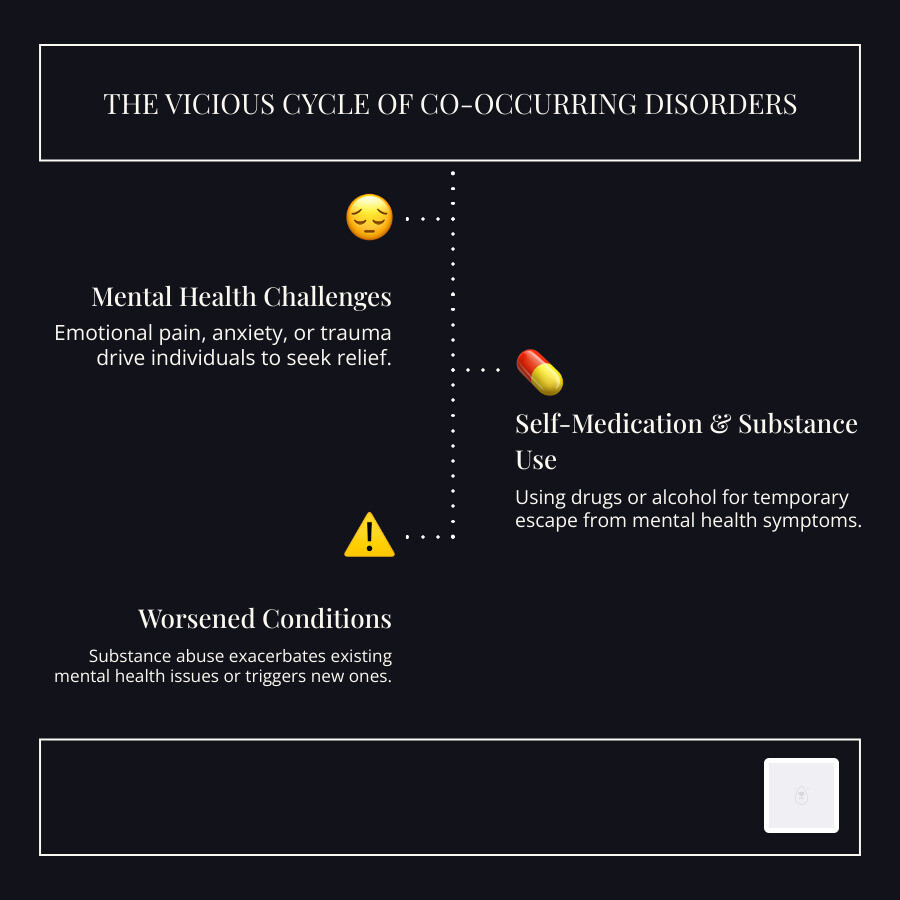
This interplay creates a vicious cycle. Mental health issues can drive individuals to self-medicate with drugs or alcohol, seeking temporary relief from emotional pain, anxiety, or trauma. Conversely, substance abuse can exacerbate existing mental health conditions, trigger new ones, or make symptoms more severe and difficult to manage. For instance, chronic alcohol use can worsen depression, while stimulant abuse can intensify anxiety or trigger manic episodes in individuals with bipolar disorder. This cyclical relationship makes recovery incredibly challenging if only one aspect is addressed.
Traditionally, treatment approaches often separated addiction and mental health care, treating them sequentially or in parallel but without true integration. This fragmented approach frequently led to incomplete recovery, higher relapse rates, and a feeling of being misunderstood by treatment providers. If the underlying anxiety driving alcohol use isn't addressed, sobriety becomes precarious. If the depression caused by opioid withdrawal isn't managed effectively, the individual is likely to return to drug use.
The need for a new approach is clear. We recognize that true healing requires understanding and addressing the intricate connections between substance use and mental health. This understanding forms the foundation of integrated addiction treatment, a holistic model designed to break this vicious cycle and offer a more sustainable path to recovery.
What is Integrated Addiction Treatment?
Integrated addiction treatment, often referred to as dual diagnosis treatment, is a comprehensive approach that addresses both substance use disorders and co-occurring mental health conditions simultaneously. Unlike traditional models that might treat these issues separately or sequentially, integrated care recognizes that these conditions are deeply intertwined and must be treated as a unified whole for effective and lasting recovery.
The philosophy behind integrated care is rooted in a holistic understanding of the individual. We acknowledge that addiction is not merely a physical dependence but a complex disease influenced by biological, psychological, social, and spiritual factors. Similarly, mental health disorders are multifaceted, impacting an individual's thoughts, emotions, and behaviors. When these two areas intersect, they create a unique set of challenges that demand a specialized, coordinated response.
In a simultaneous treatment model, individuals receive care for both their substance use disorder and their mental health condition from the same team of professionals, within the same program, and often at the same time. This ensures that treatment plans are cohesive, consistent, and mutually supportive, preventing conflicting advice or gaps in care that can arise when conditions are treated in isolation.
Consider the following comparison:
Feature Integrated Treatment Sequential/Parallel Treatment Approach Simultaneous, coordinated care for both conditions Treats conditions one after another or in separate programs Treatment Team Multidisciplinary team collaborates on both issues Separate teams for addiction and mental health Philosophy Holistic, recognizing interconnectedness Often fragmented, focusing on single diagnosis Patient Experience Unified, consistent, fewer transitions Potentially confusing, conflicting advice, higher dropout risk Effectiveness Higher success rates, lower relapse rates Lower success rates, higher relapse rates Addressing Root Causes Explores how each condition impacts the other May miss critical links between conditions By addressing root causes, integrated treatment digs into the underlying factors that contribute to both addiction and mental health struggles. This might include trauma, chronic stress, genetic predispositions, social pressures, or unresolved emotional issues. By identifying and working through these foundational elements, individuals can develop healthier coping mechanisms and build a more resilient recovery.
Integrated addiction treatment is deeply patient-centered. It recognizes the unique needs and experiences of each individual, tailoring treatment plans to fit their specific diagnoses, life circumstances, and recovery goals. This personalized approach fosters a sense of trust and engagement, empowering individuals to take an active role in their healing journey.
Why Integrated Addiction Treatment is Crucial for Co-Occurring Disorders
The benefits of integrated addiction treatment are profound, particularly for individuals navigating the complexities of co-occurring disorders. We have observed that this unified approach yields significantly improved outcomes compared to traditional, siloed treatment models.
Firstly, integrated care leads to improved outcomes across the board. When both the mental health disorder and the substance use disorder are treated concurrently, individuals are more likely to achieve and maintain sobriety, experience a reduction in mental health symptoms, and improve their overall functioning. This is because the treatment for one condition can positively impact the other, creating a synergistic effect that accelerates healing.
Secondly, we see a notable reduction in relapse rates. A common pitfall in sequential treatment is that addressing only the addiction leaves the underlying mental health issues unaddressed, creating a powerful trigger for relapse. Similarly, treating a mental health disorder without acknowledging substance use can undermine therapeutic progress. Integrated treatment equips individuals with coping strategies for both conditions, strengthening their resilience against relapse.
Integrated treatment can also be more cost-effective in the long run. While the initial investment might seem substantial, preventing relapses and reducing the need for repeated treatment episodes ultimately saves resources. More importantly, it saves individuals from the devastating personal and financial costs associated with chronic addiction and untreated mental illness.
One of the most critical aspects integrated treatment addresses is self-medication. Many individuals turn to drugs or alcohol to cope with uncomfortable mental health symptoms like anxiety, depression, or the effects of trauma. Integrated care provides healthier, evidence-based alternatives for managing these symptoms, teaching individuals effective coping skills and offering appropriate medication management when necessary. This breaks the cycle of self-medication and empowers individuals to manage their mental health constructively.
By simultaneously addressing both conditions, integrated treatment actively works to break the cycle where each disorder exacerbates the other. It helps individuals understand how their mental health affects their substance use and vice versa, fostering self-awareness and empowering them to make healthier choices.
The goal is an improved quality of life. Individuals in integrated treatment report better overall well-being, stronger relationships, greater stability, and a renewed sense of purpose. They are better equipped to steer life's challenges, pursue their goals, and build a fulfilling life in recovery.
Common Co-Occurring Disorders
The combinations of mental health disorders and substance use disorders are diverse, each presenting unique challenges that integrated treatment is designed to address. Here are some of the most common pairings we encounter:
- Depression and Alcoholism: Alcohol, a depressant, can temporarily numb feelings of sadness or hopelessness, but chronic use often worsens depressive symptoms, creating a self-perpetuating cycle.
- Anxiety and Benzodiazepine Use: Benzodiazepines (e.g., Xanax, Klonopin) are prescribed for anxiety, but their addictive potential means individuals can quickly develop dependence, leading to increased anxiety during withdrawal and a need for higher doses.
- PTSD and Opioid Addiction: Individuals with Post-Traumatic Stress Disorder (PTSD) may use opioids to escape traumatic memories or numb emotional pain, leading to addiction and further complicating trauma recovery.
- Bipolar Disorder and Stimulant Abuse: The mood swings of bipolar disorder can lead individuals to use stimulants (e.g., methamphetamine, cocaine) during depressive phases to boost energy or during manic phases to intensify feelings, often resulting in severe consequences.
- Schizophrenia and Polysubstance Use: Individuals with schizophrenia may use multiple substances to cope with distressing symptoms like hallucinations or delusions, or to manage the side effects of psychiatric medications, complicating their already severe mental health condition.
Core Components of a Comprehensive Program
A truly effective integrated addiction treatment program is built upon a foundation of comprehensive care, often structured as a continuum of services. This ensures that individuals receive the appropriate level of support at each stage of their recovery journey, adapting as their needs evolve.
The first critical step for many is medical detox. This supervised process safely manages withdrawal symptoms as the body rids itself of drugs and alcohol. Detox can be physically and psychologically challenging, and attempting it without medical supervision can be dangerous, even life-threatening, especially for substances like alcohol and benzodiazepines. In Johnson City, and across Tennessee, medically assisted detox practices are crucial for a safe and stable start to recovery.
Following detox, individuals often transition to inpatient or residential care. This level of treatment provides a structured, supportive environment with 24/7 supervision. Clients live at the facility, engaging in intensive therapy, educational sessions, and recreational activities designed to foster healing and personal growth. This immersive setting allows individuals to step away from triggers and distractions, focusing entirely on their recovery.
For those who do not require 24/7 supervision or are transitioning from inpatient care, outpatient programs offer varying levels of intensity:
- Partial Hospitalization Programs (PHPs): These programs provide intensive treatment during the day, similar to inpatient care, but allow clients to return home in the evenings. PHPs offer a structured schedule of therapy, group sessions, and medical monitoring, making them a strong option for individuals needing significant support while maintaining some connection to their home environment.
- Intensive Outpatient Programs (IOPs): IOPs are a step down from PHPs, offering fewer hours of treatment per week but still providing structured therapy multiple times a week. They are ideal for individuals who have achieved some stability but still require regular support and skill-building to steer daily life challenges.
- Standard Outpatient Programs (OPs): These are the least intensive, typically involving a few hours of therapy or group sessions per week. OPs are often used for ongoing support in early recovery or as a long-term maintenance program.
Throughout all levels of care, the cornerstone of integrated treatment is the application of evidence-based therapies. These are therapeutic approaches that have been rigorously tested and proven effective through scientific research. They provide the tools and strategies necessary for individuals to understand their conditions, develop coping mechanisms, and make lasting behavioral changes.
Finally, aftercare planning is a vital component. Recovery is a lifelong journey, and a comprehensive program ensures that individuals have a robust support system in place as they transition out of formal treatment. This includes connections to community resources, ongoing therapy, support groups, and relapse prevention strategies.

Key Therapies in Integrated Addiction Treatment
Integrated addiction treatment leverages a range of therapeutic modalities to address the complex interplay of substance use and mental health disorders. These therapies are often delivered in individual, group, and family settings, providing a multifaceted approach to healing.
- Cognitive Behavioral Therapy (CBT): A highly effective therapy for both addiction and many mental health conditions (like depression and anxiety), CBT helps individuals identify and challenge negative thought patterns and behaviors that contribute to their struggles. By learning to reframe unhelpful thoughts and develop healthier coping strategies, clients can break free from destructive cycles.
- Dialectical Behavior Therapy (DBT): Often used for individuals with intense emotional dysregulation, self-harm behaviors, and co-occurring disorders like Borderline Personality Disorder, DBT teaches skills in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. These skills are invaluable for managing cravings, intense emotions, and navigating challenging relationships in recovery.
- Individual Psychotherapy: One-on-one sessions with a therapist provide a safe and confidential space for individuals to explore the root causes of their addiction and mental health issues, process past traumas, develop personal insights, and set individualized recovery goals. This personalized attention is crucial for addressing specific needs and challenges.
- Group Therapy: Group sessions offer a powerful sense of community and shared experience. Participants learn from each other, practice new coping skills in a supportive environment, and realize they are not alone in their struggles. Group therapy fosters accountability and provides a platform for peer support, which is a cornerstone of recovery.
- Family Counseling: Addiction and mental health disorders impact the entire family system. Family counseling helps family members understand the dynamics of addiction, improve communication, set healthy boundaries, and heal from the effects of the disorders. It can be instrumental in building a supportive home environment conducive to long-term recovery.
- Trauma-Informed Care: Recognizing that many individuals with co-occurring disorders have experienced trauma, this approach integrates an understanding of trauma's impact into all aspects of treatment. It focuses on creating a safe environment, avoiding re-traumatization, and empowering individuals to process their experiences in a healing way, without necessarily requiring them to relive the trauma.
The Role of Medication and Holistic Practices
In addition to psychotherapy, integrated treatment often incorporates medication and holistic practices to support recovery. This comprehensive approach acknowledges that healing encompasses the mind, body, and spirit.
Medication-Assisted Treatment (MAT): For certain substance use disorders, particularly opioid and alcohol addiction, MAT is an evidence-based approach that combines FDA-approved medications with counseling and behavioral therapies.
- Suboxone (buprenorphine/naloxone): Used primarily for opioid use disorder, Suboxone helps reduce cravings and withdrawal symptoms, allowing individuals to focus on therapy and recovery without the constant distraction of physical dependence.
- Methadone: Another medication for opioid use disorder, methadone is typically administered in specialized clinics and helps stabilize individuals, reduce illicit opioid use, and improve overall health and social functioning.
- Psychiatric medications: For co-occurring mental health disorders, appropriate psychiatric medications (e.g., antidepressants, anti-anxiety medications, mood stabilizers) can significantly alleviate symptoms, making it easier for individuals to engage in therapy and develop coping skills. These medications are carefully prescribed and monitored by medical professionals as part of the integrated treatment plan.
Holistic Therapies: Integrated programs also accept a variety of holistic practices that support overall well-being and complement traditional therapies. These practices help individuals connect with their inner resources, reduce stress, and promote a sense of balance.
- Yoga: Combining physical postures, breathing exercises, and meditation, yoga can reduce stress, improve mood, and improve self-awareness, fostering a deeper connection between mind and body.
- Mindfulness: Mindfulness practices, such as meditation, teach individuals to be present and observe their thoughts and feelings without judgment. This skill is invaluable for managing cravings, reducing anxiety, and developing emotional regulation.
- Nutrition Counseling: A healthy diet plays a crucial role in physical and mental health. Nutrition counseling helps individuals understand how food impacts their mood, energy levels, and overall well-being, guiding them towards healthier eating habits that support recovery.
By combining the best of evidence-based therapies, appropriate medication, and supportive holistic practices, integrated treatment offers a powerful and personalized path to healing for individuals with co-occurring disorders.
The Benefits of a Unified Treatment Approach
Embracing a unified treatment approach for co-occurring disorders offers a multitude of advantages that significantly improve the recovery journey. We have seen how this integrated model transforms lives, providing individuals with the tools and support needed for lasting change.
One of the most striking benefits is higher engagement rates. When individuals feel that all aspects of their struggle are being addressed, they are more likely to commit to and actively participate in their treatment. This comprehensive understanding fosters trust and reduces the feeling that one problem is being prioritized over another, which can be a common frustration in fragmented care.
This increased engagement directly contributes to better long-term recovery. By simultaneously tackling both the addiction and the mental health disorder, integrated treatment builds a more robust foundation for sobriety and mental well-being. Individuals develop a deeper understanding of how their conditions interact, allowing them to anticipate challenges and apply integrated coping strategies.
Integrated care also facilitates comprehensive skill development for both disorders. Clients learn specific techniques for managing cravings and triggers related to substance use, alongside strategies for regulating emotions, challenging negative thoughts, and improving interpersonal relationships, which are critical for mental health stability. This dual skill set empowers them to steer life's complexities more effectively.
Moreover, integrated programs strive to create a supportive, non-judgmental environment. This is paramount for individuals who may carry significant shame or stigma associated with both their addiction and mental health issues. In such an environment, clients feel safe to share their experiences, explore vulnerabilities, and receive compassionate guidance from a team that understands the intricate nature of their challenges.
Finally, integrated treatment places a strong emphasis on relapse prevention strategies. These strategies are custom to address both substance use triggers and mental health exacerbations. Clients learn to identify early warning signs, develop personalized action plans, and build a strong support network to maintain their recovery.
Recognizing the need for dual diagnosis treatment can be the first step towards a more effective path to healing. Here are some signs that someone may need to seek integrated care:
- Using substances to cope with mental health symptoms (e.g., anxiety, depression, trauma).
- Mental health symptoms worsening during or after substance use.
- A history of multiple relapses despite receiving treatment for only one condition.
- Difficulty managing emotions or stress without resorting to substance use.
- Experiencing withdrawal symptoms from substances that also trigger severe mental health distress.
- Feeling misunderstood or that their treatment isn't fully addressing all their issues.
- A family history of both addiction and mental illness.
Long-Term vs. Short-Term Program Effectiveness
When considering treatment options, understanding the difference between long-term and short-term programs is crucial, especially for co-occurring disorders. While short-term interventions like detox are essential initial steps, their limitations become apparent when viewed against the backdrop of lasting recovery.
Short-term detox is a vital first phase, safely managing acute withdrawal symptoms and stabilizing the individual physically. However, detox alone is not a treatment for addiction or co-occurring mental health disorders. It addresses the physical dependence but does not equip individuals with the psychological tools, coping mechanisms, or behavioral changes necessary for sustained sobriety. Without follow-up care, individuals who only complete detox face a very high risk of relapse.
For individuals with co-occurring disorders, a long-term residential care program often provides the most robust foundation for healing. These programs, typically lasting 30, 60, 90 days, or even longer, offer an immersive and comprehensive treatment experience. The extended duration allows for:
- Deeper Therapeutic Work: More time to engage in individual and group therapies, process trauma, address underlying mental health conditions, and develop insight into the roots of their struggles.
- Skill Acquisition and Practice: Ample opportunity to learn and practice new coping strategies, emotional regulation techniques, and relapse prevention skills in a safe, structured environment before returning to daily life stressors.
- Behavioral Change Integration: The time needed to consistently apply new behaviors and thought patterns, allowing them to become more ingrained and sustainable.
- Stabilization of Mental Health: For those with mental health disorders, a longer stay allows for medication adjustments, consistent psychiatric care, and the development of stable routines that support mental well-being.
The goal of these extended programs is not just to achieve initial sobriety but to help individuals build coping mechanisms that can withstand the pressures of everyday life. It's about empowering them to manage triggers, steer difficult emotions, and maintain mental stability without resorting to substance use. By providing a comprehensive and sustained period of care, long-term programs significantly increase the likelihood of creating lasting behavioral change and fostering a truly integrated recovery.
Finding the Right Integrated Treatment Program
Starting on the journey to recovery for co-occurring disorders requires finding the right integrated treatment program. This decision is one of the most important you'll make, and approach it with careful consideration.
When evaluating potential programs, we emphasize the importance of verifying credentials. Look for facilities accredited by reputable organizations such as the Commission on Accreditation of Rehabilitation Facilities (CARF) or The Joint Commission. These accreditations signify that a program meets rigorous standards for quality of care, safety, and ethical practices. Such certifications assure you that the facility adheres to best practices in both addiction and mental health treatment.
Equally important are staff qualifications. An integrated treatment program should employ a multidisciplinary team of licensed and experienced professionals, including addiction specialists, psychiatrists, psychologists, therapists (with expertise in CBT, DBT, trauma-informed care, etc.), medical doctors, and nurses. Inquire about their experience specifically with co-occurring disorders.
A hallmark of effective integrated treatment is the development of individualized treatment plans. No two individuals are alike, and a one-size-fits-all approach is rarely effective for complex conditions. The program should conduct thorough assessments to understand your unique needs, diagnoses, history, and goals, then tailor a plan that evolves with your progress.
Understanding the admission process overview is also key. A transparent and supportive admissions team can guide you through the initial inquiry, assessment, insurance verification, and intake procedures, making the transition into treatment as smooth as possible.
Communities across the nation are seeing a rise in specialized care, with options for Integrated Addiction Treatment Johnson City and other areas providing comprehensive services. Seeking out such specialized centers ensures that you receive the coordinated care necessary for both your substance use disorder and any co-occurring mental health conditions.
How to Pay for Treatment
Concerns about the cost of treatment should never be a barrier to seeking help. We understand that navigating the financial aspects of drug rehab in Johnson City or elsewhere can be daunting, but numerous options are available.
- Navigating Health Insurance: The federal Mental Health Parity and Addiction Equity Act (MHPAEA) mandates that most health insurance plans must provide coverage for mental health and substance use disorder treatment at the same level as medical and surgical care. This means your private insurance plan should cover a significant portion of your integrated treatment. It's crucial to contact your insurance provider directly to understand your specific benefits, deductibles, co-pays, and in-network vs. out-of-network coverage. Many treatment centers also offer insurance verification services to help you understand your coverage.
- State-Funded Programs (Medicaid): For eligible individuals, TennCare, Tennessee's Medicaid program, can provide coverage for addiction and mental health treatment. Eligibility typically depends on income, family size, and other criteria. TennCare may cover various levels of care, including detox, inpatient, and outpatient services, making treatment accessible for those with limited financial resources.
- Medicare Coverage: Individuals aged 65 or older, or those with certain disabilities, may be covered by Medicare. Medicare parts A and B can cover inpatient and outpatient mental health and substance use disorder services, respectively. Coverage details can vary, so it's important to confirm with the treatment facility and Medicare directly.
- Sliding Scale Fees: Many treatment centers offer sliding scale fees, where the cost of treatment is adjusted based on an individual's income and ability to pay. This option requires providing proof of income and can significantly reduce the financial burden, making quality care more affordable.
- Private Pay Options: For those without insurance or who prefer not to use it, private pay allows individuals to cover the cost of treatment out-of-pocket. While this can be a significant expense, it offers flexibility in choosing providers and programs without insurance restrictions. Some facilities may offer payment plans or financing options.
Don't let financial concerns deter you from seeking the help you need. Most reputable treatment centers have dedicated admissions or financial counselors who can help you explore all available payment options and find a solution that works for you.
Legal Protections and Support Systems
Beyond the clinical aspects of treatment, understanding the legal protections and robust support systems available in Tennessee, particularly in areas like Johnson City, can provide immense comfort and practical assistance during recovery. We believe that a strong community and supportive legal framework are integral to a successful healing journey.
Tennessee has implemented several progressive laws designed to encourage individuals to seek help and reduce the harms associated with substance use. The Good Samaritan Overdose Prevention Act, enacted in 2014, is a critical piece of legislation. It provides immunity from civil suits for naloxone prescribers and grants civil immunity for individuals who administer naloxone during an overdose. Crucially, it also protects individuals who call for help during an overdose from being arrested or prosecuted for drug possession. This law aims to remove the fear of legal repercussions, encouraging people to save lives.
Furthermore, Tennessee offers alternatives to incarceration through drug court programs and the Tennessee Drug Treatment Instead of Incarceration Act. These initiatives allow nonviolent drug offenders to participate in comprehensive rehab programs instead of serving jail time. Successful completion of treatment often leads to the dismissal of charges, offering a pathway to recovery and reintegration into society rather than perpetuating the cycle of incarceration.
For ongoing support, peer support specialists play an invaluable role. These individuals have lived experience in recovery and are trained to provide guidance, encouragement, and mentorship to others. They offer a unique perspective, fostering hope and demonstrating that recovery is achievable. Many local resources in Johnson City and the surrounding areas offer peer support services, connecting individuals with mentors who understand their journey.
Mutual aid groups are another cornerstone of long-term recovery. Organizations like Alcoholics Anonymous (AA), Narcotics Anonymous (NA), and SMART Recovery provide free, accessible meetings where individuals can share their experiences, build community, and gain strength from their peers. These groups offer a continuous source of support, accountability, and fellowship, which are essential for maintaining sobriety and mental well-being over time.
The importance of community cannot be overstated. A supportive network of family, friends, and fellow individuals in recovery creates a vital safety net. It provides emotional encouragement, practical assistance, and a sense of belonging that combats isolation—a common trigger for relapse. Local resources and community centers in Johnson City often facilitate connections to these crucial support networks, ensuring that individuals never feel alone on their path to healing.
By understanding and utilizing these legal protections and support systems, individuals in Johnson City and across Tennessee can find a more secure and supported path through integrated addiction and mental health treatment toward lasting recovery.



No comments:
Post a Comment
I love reading and responding to comments but in order to get my reply you must ensure you are NOT a no-reply blogger. If you are, here are some quick steps to change that!
1. Go to the home page of your Blogger account.
2. Select the drop down beside your name on the top right corner and choose Blogger Profile.
3. Select Edit Profile at the top right.
4. Select the Show My Email Address box.
5. Hit Save Profile.